The symptoms got worse ...
I was young (31), fit, and healthy and went to see my GP about some bleeding and pains in my rectum. I didn’t think too much about it initially, and it was unusual for me to visit the doctor as I’d hardly visited much in life prior to this.
Despite the bleeding, it was suggested that it could be piles or haemorrhoids. I went away but the symptoms got worse, and I started seeing more bleeding and increased pain. When I went back again they checked my bloods, which were fine, so was advised to see if symptoms persisted (which they did).
I frequently visited the Doctor and wanted to be referred, it all took too long. I was finally seen for a colonoscopy and as soon as the camera was inserted they realised there was a large tumour in my rectum. They took a biopsy and then told my wife Cherida and I the news that it was bowel cancer on the same day. A day we will never forget and one that just shattered our lives completely.
Danny grew up in North Wales however, at the time of his diagnosis, had recently moved to Oswestry. His early treatment involved daily trips for Radiotherapy at Glan Clywd, the North Wales Cancer Centre. He made the hour-long journey every day for five weeks driving backwards and forwards. The only positive being the outbreak of the Covid pandemic meaning there was no traffic on the roads.

I had 25 rounds of radiotherapy and then a scan at the end of May and they said the tumour had shrunk, we were obviously pleased to hear that. I was referred to Christies in Manchester for an operation to remove the tumour, all my information was sent there, and I had further, full-body scans, which unfortunately led them to find further metastases on my liver, which is apparently common with bowel cancer. I started chemotherapy in August 2020, and was scheduled for eight sessions, but after five sessions Christies reviewed my results and the tumour in my rectum had shrunk enough and left clear margins, they stopped chemotherapy to prepare me for surgery.
Surgery to remove the tumour was initially scheduled for the end of 2020 but was pushed back to January 2021. Surgeons removed 100% of the tumour and Danny was given a permanent stoma. Following months of recuperation at home he was given a further scan which showed his bowel and liver were now clear. But another full body scan at Christies revealed he had cancer on his lungs.
The chemotherapy drugs had some really awful side effects
I lost over a stone during the operation to remove the tumour, my organs didn’t want to restart and I was in Christies for nearly three weeks. It was really hard during Covid and I wasn’t allowed to see any visitors, not even my wife. I had to learn to walk again which is something I never ever thought I would have to conquer at 32 years old. I’ve got a permanent stoma now and it’s a big life adjustment to say the least. I was told when I got diagnosed I would have to have one because the tumour was in an awkward place.
A full body scan in April 2021 found metastases on the right lung, it had spread from the primary bowel site, as well as to my scapula (although inconclusive) and liver. So I had more chemotherapy starting in May 2021. I started a course of 12 rounds of intense chemotherapy which lasted to October 21. It was gruelling, extremely difficult. My digestive system was very different because of the stoma which made things even more complicated. The chemotherapy drugs had some really awful side effects. I had a very severe chemotherapy rash, spots and blisters all over me. It was instantaneous.

I became really sensitive to the light so I had to stay inside, I wasn’t allowed in the sun. It was so disheartening because I love to be outside, but this wasn’t advised on warm days. Covid was still at its peak and I hadn’t had any vaccinations. Consultants couldn’t guarantee I would be ok with any new vaccinations in case it interfered with my treatment, so I waited a while to have any, therefore I really did have to stay inside and isolate.
Danny was told that his treatment would affect his fertility and so the couple decided to pursue IVF. Storage of his sperm was arranged in Manchester Hospital and at The Royal Shrewsbury prior to radiotherapy taking place. They have had two attempts – one through the NHS, one privately – sadly neither have so far been successful, but they intend to keep trying. Understandably this is added distress on top of everything else the young couple have been faced with.
In February 2022 Daniel started a new job as a Principal Utilities Engineer with a Master Developer. A scan in April 2022 revealed some of the cancer had started to grow back so he underwent a further 12 rounds of chemotherapy before undergoing a phased return to work.
Daniel is half-Jamaican and has had tests to see if his cancer is genetic – both his Dad and paternal Grandma are Jamaican and underwent their own cancer experience. If the results prove Daniel’s cancer is genetic he and his wife will be eligible for another source of fertility treatment, which is exclusive to those with genetic conditions.
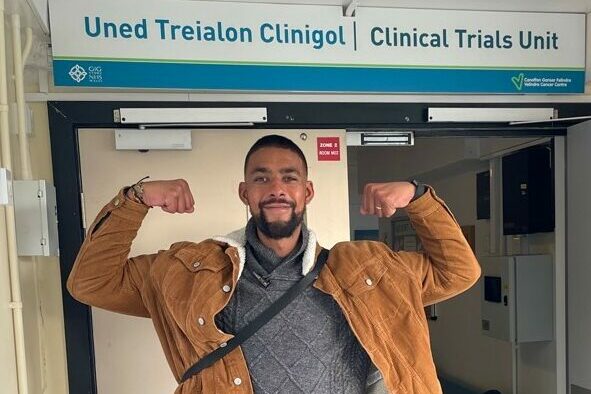
Because I grew up in Wales and it was in Wrexham that I had my original diagnosis, I am part of the Welsh healthcare system. I’ve been invited down to Cardiff to participate in a clinical trial, whereby I understand I am the only patient in Wales currently enrolled on this particular trial.
It’s very interesting, and involves a combination of immunotherapy and clinical drugs. The sessions are weekly, and require my wife and I to spend three days per week in Cardiff. Clinical trials can be fantastic, the treatment is far more specific and it’s tailored to my specific cancer mutation and cell behaviour.
Life changing
When, in January 2021, surgeons removed Daniel’s bowel and he was given a permanent stoma he says it really was a life-changing thing. He has gone on to learn how to manage it and new routines, and is now passionate about helping other people who have stomas for whatever reason.
He was supported by staff at his local GP Clinic in Oswestry and inspired the creation of a new service available to all patients living with cancer in Shropshire and Mid Wales.
It took some time adapting to having a stoma and I was at home for a few months of recovery. We didn’t venture out too far and I was learning how to walk again. We tried going a bit further when I was up to it, just for take-away coffees but I wasn’t comfortable going any distance.
I was introduced to Val McKay and brought up the lack of changing facilities for people with a stoma. Public toilets just aren’t acceptable. I never had to think about things like this before but now I was worrying about where I could change that was hygienic enough. It became quite apparent that there just wasn’t many suitable options.
Although it has taken a long time to adjust to my new bowel habits, I’m used to my stoma now and have a good routine, I’m quite fortunate. But I’m sure there are people who are anxious about travelling and going places because they’re not sure about where decent facilities are. Val explained about the radar keys and as soon as I was given one it was great. I’m not an anxious person but being able to access larger, better looked after public facilities made it a lot better for me.
I’ve noticed these kind of toilets around more now, I’ve never needed disabled toilets before but now I do, and now I can access them it’s great. We went to Edinburgh for our five year wedding anniversary last year. It was just what we needed, and there were lots of facilities I was able to access with the radar key. It’s the furthest I’d been since I had my stoma and it was good to be able to use it up in Scotland.
People wouldn’t look at me and think I’m a cancer patient. I do find that people look at me using disabled facilities and I can tell they think I’m not supposed to be in there. It’s not a disability, but it’s very close. It’s a life-changing adjustment, I’ve had to make big changes, physically as well as mentally, and had no choice but to come to terms with the fact that I will not be the same again. I feel sad for people who are older and alone, and those who are young and perhaps single, it will really impact their confidence, because there’s a lot to learn and it changes your physical appearance. You have to think about different clothing and swimwear. You also have to think about gas and how you can’t control the movements or sounds!
It’s important to plan and be organised, really take note of your diet and make sure you always have supplies to hand, it’s just getting into a routine with it all and unfortunately learning as you go from mishaps that do arise along the way.
Daniel has recently returned from a long holiday to visit some family in Jamaica. He is looking forward to being involved in the Welsh clinical trials, moving on with further fertility treatment, and continuing to live his life as best he can.
I was diagnosed with cancer at 31 and instantly became very angry and upset because I look around and see people not living healthily and taking care of themselves and I think ‘why me?’ I didn’t really drink, I didn’t smoke, and I was big into fitness. I also adopted a plant-based diet around seven years ago so it’s very frustrating to be in this situation now.
Hearing you have cancer is just the worst possible news to have to deal with and then accept, it’s just something I never thought would happen to me.
I know how scary it all is for people who are diagnosed and everything that is associated with it, the fear, the unknown, the constant dark cloud that follows you around everywhere that can’t be shaken off, but you can still enjoy yourself and be you if you find the positives in everyday, it doesn’t matter how small.

May 23
I’m now going to Cardiff every week Monday to Wednesday, it’s very intense, but important to be a part of trial. It’s called the intrinsic clinical trial, with early-stage drugs being trialled for my particular cancer mutation. I do fasted blood tests on a Monday and doctors will examine me. A Tuesday is a full day of treatment and further examinations. I have IV drugs and the clinical trial drug, it’s a combination treatment. The IV drug is supposed to stick to the cancer cells so they don’t move and multiply, and the clinical drug kills them. On a Wednesday I recover and then we make the three-hour journey back home.
I’m the only active participant on this particular trial at the moment, I’m very well looked after by the Consultants, Doctors and Nurses. I have to have lots of blood work, which all depend on what cycle of the trial it is on. I have to check my blood sugars every day because there’s a risk of diabetes, but so far it has stayed within a healthy range.
I had quite an instantaneous reaction to the drugs and developed the chemo rash (again!), so they had to stop the clinical drug for a couple of weeks until it moved down a grade, but kept me on the immunotherapy IV during this process. I have a daily routine to apply plenty of creams and tablets to stay on top of the rash, but it is triggered with both the IV drug and the clinical drug, so it’s a weekly battle.
I’m keeping my eye on work when I can and I’m extremely grateful to my employer for their continued support. Having not long joined the company before having to embark on further treatment, they have been nothing short of fantastic. This isn’t something we take lightly and I am very aware how rare this support is during cancer treatment from employers, having spoken to other patients who seemingly do not receive this, and I appreciate it beyond measure.
We are very lucky to have such a great support network from our friends and family, who have been crucial in helping us to navigate this journey. Life would be even more difficult without them.
Autumn 2024
In 2023 Danny was invited to join a clinical trial in Cardiff, initially he saw some good initial results but then the drugs stopped working effectively.
More recently he has undergone ablation treatment – a process that uses electrical energy and heat to destroy cancer cells. Danny spoke to Lingen Davies with the latest on his experience…
The drugs stopped working...
“I was still in a better place than when I started, but once the drugs stopped working they had to stop the trial. That was a shame because things were initially moving in the right direction. When the clinical trial stopped I went back to the oncology team for further assessment and unfortunately, further chemotherapy”
“It was all quite disheartening. You hear about people having amazing results from clinical trials, and it didn’t work as we had wanted. With clinical trials, they are clearly still in the early development stages and given the low number of active participants (think I was the only one in Cardiff) they were pleased I was eligible and a good fit for the trial.”

Trialling new treatment options
Danny returned to being treated through teams in Wrexham, with consultants still on hand from the Christies. Specialists at Aintree Hospital also contacted him after seeing recent scans that had been shared. The metastases were still relatively small and hadn’t changed much since he was first approached by Aintree a couple of years prior. Seeing how he had continued to respond to treatment, it was advised that he would be a good fit for ablation treatment.
“In September last year one of the Doctors, Professor Rob Jones at Aintree, discussed with us the potential use of ablation, which is a relatively new treatment, this was subject to further detailed scans and a full body bone scan. This treatment was mentioned to me previously however, as we were under the impression I had some disease in my scapula (bone) it was ruled out. Ablation is effectively inserting a small needle through to the affected site, it is done under a general anaesthetic and they do it under a live CT scan, to ensure they treat any disease which is visible. They make multiple incisions and microwave the tumours, 96 times out of a 100 the metastases don’t come back.”
Danny had full body scans done in Aintree and started chemotherapy again in October 2024, to keep everything in hand ahead of the ablation and it was recommended that a further 6 rounds of chemotherapy should shrink the disease enough, to ensure that ablation was appropriate. This time for the chemotherapy, he was fitted with a portacath which is inserted under the skin and allows for the treatment to be taken directly from the main vein, rather than a picc line or a cannula. This allowed much better range of movement and allowed him stay active during treatment.
Danny had his initial ablation in February after which he felt very bruised and took a few weeks to recover. There are two different types of ablation which essentially microwaves the metastases away and it’s all done on a day admission basis.
“They made incisions all over my front and back, it was quite hard to sleep!”
Six weeks after the ablation he had another scan which showed all the ablation sites were scar tissue (melted), which was good news. A separate area of metastases on his lung and liver was identified at the scan and a further ablation session was scheduled for June.
“I only had two incisions in June, as they were the small ones which could’ve been missed during the first ablation procedure. Thankfully, the recovery was a bit easier. Ablation is preferable to chemotherapy, it means I can stay fit and keep more active, it also doesn’t come with some of the unpleasant side effects of traditional treatment. My body is still a little sensitive where the sites have been (lungs and liver), but I am grateful to have had them done.

To date Danny has undergone 86 rounds of treatment – 25 radiotherapy, 25 immunotherapy, 36 chemotherapy, one operation, and two ablations. Despite everything he remains positive and is using his lived experience in his new role on the Lingen Davies Board of Trustees.
His latest scan results (September 2024) showed that there was no new disease and that the ablated sites were just shown as scar tissue, which is fantastic news. He is due for more scans soon.
Danny and his Wife, Cherida – are hoping to have another round of IVF in the new year (it will be Cherida’s fourth) as they are still really wanting to start their own family and move forward with their lives.
Danny has kindly given his time to supporting our Bins for Boys project. He is passionate about highlighting the situation for many men like him who are left with ongoing health issues as a result of their cancer treatment.
Read more about our Bins for Boys project here and find out how you can involved.
